My mother is in a COVID isolation ward in Morriston Hospital in South Wales. COVID really knocked her out but she was mostly back to normal when I visited on Sunday (26th Oct 2025), which is a relief. The air quality in a room specifically set aside for patients infected with an disease that spreads across the air, is however pretty depressing.
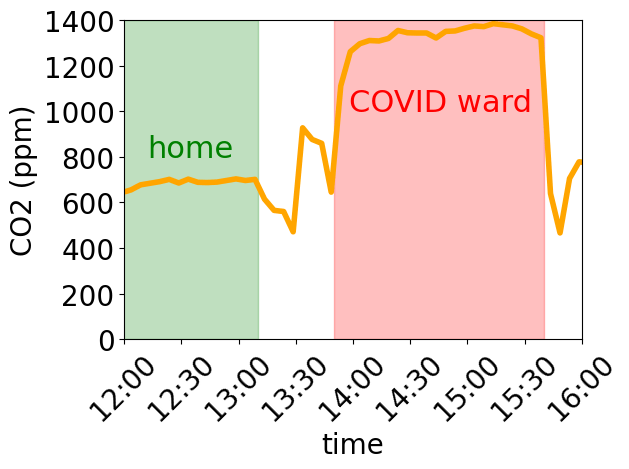
The plot* shows a proxy for air quality – the concentration of CO2 (carbon dioxide) – as a function of time for part of my Sunday. The green-shaded area was when I was at home before I visited my mum, and the red-shaded area is the hospital visit.
Fresh outside air has a bit more than 400 ppm (parts per million) CO2. I waited outside the hospital for an Uber for a few minutes at around a quarter to four, and you can see that the CO2 concentration dips to around that level around that time.
Earlier in the day at home (12 to 1 pm), the CO2 sensor was in a well ventilated room at home and so the CO2 was only a bit above 600 ppm. The excess CO2 came from me, we all breathe out CO2 as part of our natural metabolism.
However, in the ward with 6 patients recovering from COVID, plus staff and visitors, the CO2 level was over 1200 ppm. A consensus set of recommendations published in Science by over 40 scientists and engineers including many real leaders of the field, recommended that the CO2 level be kept below 800 ppm.
Morriston Hospital and NHS Wales have not listened to these very well informed people. I think this matters. The maths of this is easy.
For every roughly 400 ppm above the background outside level, the air contains an extra 1 % of second-hand air. By coincidence the background around 400 ppm. So for example, 600 ppm is only around 200 ppm above the background. So air at home is roughly 99.5% fresh and only 0.5% second hand. If I have caught COVID**, and if a visitor popped round then only 0.5% of the air the visitor would breathe in has passed through my lungs and so may have picked up a virus.
However, at 1200 ppm, 2% of the air in the COVID ward has been through someone’s lungs. In this case mainly through the lungs of COVID patients***. This is not ideal for hospital staff and visitors. With decent ventilation, this could be halved, making the room safer for the nurses, doctors, other staff, and visitors.
This is disappointing. I am happy to believe that Morriston Hospital does, fir example, gall bladder operations competently and according to best practice. But not ventilation, and so not limiting COVID, flu etc disease transmission in the hospital. It is frustrating that neither senior medics doing infection control nor politicians appear to want to do more than wring their hands at waves or COVID and flu infections.
* Data and code (Python Jupyter notebook) for the plot are on github.
** Given that I have spent hours in a poorly ventilated room with people recovering from COVID, this is a real possibility of course. But at least I wore a decent mask, an FFP2, unlike the poor nurses and doctors who have to make do with much less effective surgical masks. Sigh.
*** A lot of the time there was a nurse or another healthcare worker in the ward but with 6 patients plus a visitor to two, most but not all of the CO2 would be from the patients, all of whom had been diagnosed with COVID.